Early Total Cervix Occlusion (ETCO) |
||||||||||||||||||||||||||||||||||||||
|
IntroductionRecurrent late abortions and very preterm births continue to be two of the up to now insufficiently solved problems of modern obstetrics and perinatal medicine. The patients concerned often feel heavily burdened: On the one hand they deeply long for an infant and on the other hand they experience recurrent losses, which are often accompanied by increasing psychological problems. To achieve a surviving infant in such cases is a particularly important medical and psychological task. PathophysiologyOne of the main reasons for late abortions and very preterm births (≤ 32+0 weeks) are ascending infections from the vagina (see also “Late abortions and prematurity/causes”). Therefore we advise all pregnant women to have screenings performed by a physician/midwife for disturbances of the vaginal milieu or infections on a regular basis and, furthermore, to participate in our Self-Care-Program. However for some women this is not sufficient, particularly in cases with higher risk of (recurrent) late miscarriage and very preterm birth. Cervical Insufficiency vs. Dysfunction of Cervical ClosureUnfortunately, for these cases the term “cervical insufficiency” is still often used. It would be better to talk of “dysfunction of cervical closure”. According to Ramsauer (Ramsauer 2012) there are various causes such as:
In addition, Romero et al. (2006) discuss also congenital disorders and the inhibition of progesterone action. Of course, the causes might be mutually dependent, e. g. several of the causes listed above could favor the ascension of infections. However, and taken altogether, infections play the most important role. According to Romero, among pregnant women presenting with “cervical insufficiency” the prevalence of microbial invasion of the amniotic cavity (MIAC) is 51.5 %. In this field of study further research is definitely necessary. Early Total Cervix Occlusion as preventive measureIn cases with repeated late abortions and preterm births, the Early Total Cervix Occlusion (ETCO) is the most effective measure of prevention and differs definitely from cerclage (see below). The total cervix occlusion creates a complete barrier against ascending infections within the cervical canal. We introduced this measure in 1981 (Saling 1981). Before that time in the literature there had been very few publications about a late occlusion of the cervix. The occlusion was performed almost only in cases of threatening abortions, and always when an advanced stage in the abortion process had been reached. For example, in 1961 Szendi published two articles on the subject “Prevention of advanced miscarriages and abortion through total cervix occlusion”. At that time the cervix occlusion was an emergency measure, particularly in cases with prolapse of membranes. Our approach was completely different. We introduced the cervix occlusion as a measure to prevent early labor at all. It should be performed when:
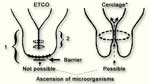
It is important to note, that the ETCO is quite different from a cerclage (and in principle also from the occasionally used pessary). Whereas the ETCO really closes the cervical canal and thereby prevents the ascension of microorganisms, the cerclage (or pessary) in contrast, only tightens the canal (fig. 1) and leads to much poorer results (see below).
Caution!
Not everything that is called “cervix occlusion” is actually a cervix occlusion according to Saling ! The portio can only grow completely together if the superficial epithelium is removed before stitching. If this is not done, then it's not a cervix occlusion according to Saling, but in effect a kind of cerclage. We would like to point out in particular that the so-called “Cervical Occlusion Trial” of the workgroup of Secher and Brix (Brix et al. 2013) is not a total occlusion but only a particularly tight form of cerclage. |
|||||||||||||||||||||||||||||||||||||
|
|
DefinitionsWith regard to the Total Cervix Occlusion (TCO) we differentiate between “early” and “late” and between “small” and “extensive” (table 1). Because the results to prevent prematurity are much better (see below) we recommend to perform the TCO “early” (ETCO) rather than “late” (LTCO). For most cases we recommend to perform the Total Cervix Occlusion as early as possible (ETCO.
Table 1: Definitions with regard to Total Cervix Occlusion (TCO) |
|||||||||||||||||||||||||||||||||||||
|
|
Indications and contraindicationsIndications for Early Total Cervix Occlusion (ETCO)
Contraindications for ETCOContraindications for ETCO are an already dilatated cervix with apparent signs of infection or labor activity which cannot be inhibited therapeutically. Indications for Late Total Cervix OcclusionOriginally, the Total Cervix Occlusion (TCO) was applied by Szendi in 1961 as a late emergency measure and can of course still be applied nowadays as secondary measure:
However, if possible the preventive (early) occlusion has absolutely to be given preference (see also further down under results). |
|||||||||||||||||||||||||||||||||||||
|
|
Scheduling the operationThe ETCO should be performed preferably between 13+0 and 24+0 weeks, and when the cervix is not yet altered. The reason for this timing is based on the intention to perform surgery not too early but to wait whether the pregnancy stays intact during its first trimester (or perhaps miscarriage occurs for some other reasons). On the other hand, ascension of infections prior to the occlusion has to be prevented as far as possible. For most cases occlusion is indicated at around 12 gw. Though, if necessary (especially in case of abortions in the patient’s history that had occurred rather early during pregnancy) the total cervix occlusion can be applied already before 12 gw. |
|||||||||||||||||||||||||||||||||||||
|
|
Preoperative measuresExaminations for infections are compulsory, for example vaginal, cervical and urethral smears with microscopic and/or bacteriologic examinations. In case of pathological findings the patient should receive an appropriate local or a systemic therapy. |
|||||||||||||||||||||||||||||||||||||
|
|
Operation techniqueInstrumentsFor the performance of the operative Total Cercix Occlusion (TCO) the usual instruments for operations at the cervix are recommended, and in addition a special loop-instrument and a device for smoothing down, which are both explained below. Figures A and B both show the instruments that are used in the Vivantes Clinic Berlin Neukölln (Berlin, Germany). Special instruments are marked.
Ligature with the loop instrumentBefore starting the operative occlusion, we highly recommend that the portio should be tied off as high as possible to prevent bleeding, in such a way that there is a nearly complete stoppage of the circulation. This measure has two decisive advantages:
We have developed a special loop instrument for this purpose (Saling and Lescinski 1989, see figs. 3 and 4).
There is a ratchet at the loop instrument on the traction stick with a blocking spring (fig. 4). This allows the stainless steel braided wire loop (fig. 3), to be attached in a circle around the portio and to be fixed up in a tightened state. We always try to clamp the loop so tight that only minimal bleeding remains. This is a sign that the tissue circulation is not completely interrupted. When the hemostasis has to be suspended at the end of the operation, the traction stick is turned about 90°. The blocking spring slides out of the traction and the loop is set free. The loop instrument can be obtained from Faromed GmbH, Berlin. Removal of the epitheliumAs mentioned above: the cervix can only grow completely together properly, when prior to the sutures the upper surface of the portio has been dissected, that is to say, the epithelium has been almost completely removed. (Otherwise, it is not a Total Cervix Occlusion after Saling, but just a form of cerclage.) Earlier, the epithelium was removed from the portio surface by sharp dissection with a scalpel, which took time. In the meantime a better method has been introduced: by smoothing down the surface of the portio with a high revving rotating simple sterile wire brush (see fig. 5a), as is used in dermatology to smooth out scars. With this method the tissue is given a considerably better and more certain chance of regeneration.
After removing the epithelium of the portio, the glandular epithelium of the cervical canal is also removed, as far as possible to a depth of about 1 to 2 cm using the same rotating device, whilst the os uteri is spread using mosquito clamps (fig. 7).
Stitching techniqueThen 2–3 inner circular stitches are made to close the cervical canal (fig. 8). Consequently two rows of knotted stitches are made, which close the outer os uteri completely (fig. 9). For all the stitching we use synthetic monofile thread like PDS. These threads, when compared to catgut, are much better for the healing process and are reabsorbed much more slowly.
|
|||||||||||||||||||||||||||||||||||||
|
|
Postoperative periodRecommendations for the time after surgeryAfter complete healing (see fig. 10) which takes approx. 2 weeks, the expectant mother may behave as any other pregnant woman (of course, as far as no other reasons speak against it).
Shortening of the cervix after ETCOIn some cases after the Early Total Cervix Occlusion (ETCO) a shortening or even funnelling of the cervix is observed. Without ETCO this would be taken as risk predictor for a threatening preterm delivery. However, experience has shown that after ETCO the shortening is not of relevance. ** |
|||||||||||||||||||||||||||||||||||||
|
|
Measures at the end of pregnancyIn the late phase of the pregnancy the outer os uteri can spontaneously have opened already slightly. Some colleagues have already had good experiences with waiting until the scar opened by itself during labor. Then – in order to dilatate – we penetrate the loose cervical tissue in the assumed direction of the cervical canal with the finger to a depth of about 1–2 cm (fig. 11).
|
|||||||||||||||||||||||||||||||||||||
|
|
Mode of deliveryWe do not think that a primary cesarean section is
necessary at all. Quite the contrary: When a recanalization of
the cervix takes place during a vaginal delivery, this is in
fact a good prerequisite for the reestablishment of normal
anatomic conditions. In all those patients who achieved a vaginal delivery after ETCO, the epithelium tissue around the wounded area of the portio recovered during the puerperium within a short space of time (a few weeks) and it is surprising – particularly since the introduction of the gentle epithelium removal technique – how little of the operational scar is to be seen later on after regeneration during the puerperium (figs. 12 to 14)
|
|||||||||||||||||||||||||||||||||||||
|
|
ResultsTo assess the results of ETCO, particularly in comparison to the cerclage, one should only look at high-risk groups such as matching the above mentioned indications for an ETCO (≥ 2 late abortions or preterm births). We have no knowledge of any randomized study about the ETCO. On the basis of the results published so far we do not think that the operation can be withheld from any woman with such a critical history. Furthermore – at least not in Germany where ETCO has already become very popular – very likely no women would agree to being integrated into a control group of a randomized study anyway after the obligatory pre-operation discussion. Therefore an acceptable solution is to compare the outcome of pregnancies after performing an ETCO with the outcome of former pregnancies of the same patients (Saling 1984, Saling & Schumacher 1996, Hormel & Künzel 1995). We should also consider that the chances of giving birth to a surviving infant are reduced the more late abortions or preterm births the woman has previously had (McManemy et al. 2007). Results from the 1980s and 1990sIn 1990 (Giffei 1990, Saling 1990) we evaluated retrospectively the data of a group of 113 patients with previous recurrent abortions. From a total of 389 wanted pregnancies only 101 infants were born alive (26 %). However, 35 of these infants died in the neonatal period. In total 66 survived, which means that only 17 % of all these pregnancies resulted in a surviving infant. Through the introduction of the total cervical occlusion (either early or late TCO) the same patients achieved 132 pregnancies with 94 live and surviving infants (71 %). We could also show, that the results in cases with an “early” TCO are twice as good as with a “late” TCO (80 % vs. 40 %). If one considers the 38 cases where the pregnancy was unsuccessful, there were 10 newborns with an extremely low birth weight, who died shortly after birth. In the remaining cases there were abortions, 13 of which occurred after a late occlusion, and 15 after an early occlusion. So the rate of abortions after the “late” occlusion amounted to 43 % against only 15 % after the “early” occlusion (Saling 1990). Similarly good results have been obtained by other clinicians performing the TCO: In 1996 we reported the results of a multi-center-evaluation, in which 11 German hospitals took part (Saling & Schumacher 1996) and the outcome of a total of 819 pregnancies with TCO was assessed. It emerged that the rate of surviving infants in the pregnancies before TCO had been performed was 21 % compared to 74 % in the pregnancies with TCO. Hormel and Künzel (1995) reported similar good results. As far as the mode of delivery is concerned, 71 % of the patients with a cervical occlusion had a spontaneous delivery and 15 % had an operative vaginal delivery. The rate of cesarean sections was 14 % in comparison to 9 % for the whole department at that time (Saling 1990). This relatively low cesarean rate shows that in most cases after ETCO labor (after the scar has been opened) can mostly happen vaginally without any problems. This is actually recommendable, since the cervix is stretched, which can be regarded as advantageous for the regeneration process after the operative occlusion. In 1997 we reported the results of a follow-up examination carried out on 52 women who had previously had a total cervical occlusion (Saling & Schumacher 1997). On the basis of these results it can be concluded that no remarkable negative effects have been proven in connection with the operative total cervical occlusion. Latest ResultsIn later publications, e. g. from Ramsauer (2012), even better outcome numbers are reported: Ramsauer in her publication refers to the ETCO as prophylactic or “primary” cervix occlusion. Thereby for 315 pregnancies in the period 2008–2011 a success rate of 95 % could be achieved, and with the so-called secondary cervical occlusion (late TCO) still a success rate of around 90 %. ETCO versus CerclageThe cerclage – despite controversial discussions – is still a widespread measure about which numerous publications exist. Various authors report good results, but one should look at these reports very closely and verify whether or not the cerclage had been performed on women at similar high risk (see above). The cerclage – and in principle this holds also true for pessaries – is hardly capable of preventing the ascension of infections because this method only tightens the cervical canal and does not close it (fig. 1). In our sample of women who were treated with ETCO (Saling 1990) we found that in 51 previous pregnancies in which cerclage was performed, only 13 infants survived. This is a survival rate of only 26 % (as compared to a survival rate of 80 % with ETCO and of 40 % with “late” TCO). These results underline how advisable it is to give the ETCO preference over cerclage in cases with such critical history. (An extensive discussion of the various operative possibilities is to be found in Vetter and Kilavuz (2001).) Some colleagues combine the total cervix occlusion with an additional cerclage. We, however, have not found any reasons why this should be done. |
|||||||||||||||||||||||||||||||||||||
|
|
Multiple pregnancy and ETCOAll the results published up to now concern women who had already had at least one early, respectively one late abortion in the past. In the meantime very new results are available whereby ETCO was performed as a general preventive measure in multiple pregnancies (which are known to have a higher risk of prematurity), even if the women concerned had not had a poor medical history: Since 1990 Schulze (2008) has performed an ETCO as a prophylactic measure in the Women’s Hospital in Cottbus (Germany) on all multiple pregnancies – when the patient agreed with his suggestion – and has achieved remarkable success with it: From a total of 219 multiple pregnancies he performed an ETCO on 96 of the women, whereas the other 123 women did not have the operation. The rate of very preterm births – that is to say < 32 gw – was 24 % in the cases without ETCO and 13.5 % in those with ETCO. In the group of infants at extremely high risk, who were born with less than 28 completed weeks of gestation, the rate without ETCO was 4 % and with ETCO it was 1 %. Consequently the perinatal mortality in cases after ETCO was almost half as much. Without ETCO it was 4.1 % and with ETCO it was 2.5 %. When considering the existing data material, it is perhaps too early to recommend that an ETCO should be performed in all multiple pregnancies, before the good results have not been confirmed at other places. Furthermore up to now there is no study existing whether the ETCO or the Self-Care-Program for Pregnant Women is more successful in multiple pregnancies in cases without poor history.) Nevertheless such a possibility should be seriously considered – particularly in multiple pregnancies with additional risk factors (e. g. after in-vitro fertilization, or in a pregnant woman near the end of her potential reproductive time). |
|||||||||||||||||||||||||||||||||||||
|
|
ConclusionOn the basis of previous experiences and available results the Total Cervix Occlusion – in particular the early occlusion – is a convincingly efficient operative measure for the prevention of late abortions and very preterm births, particularly in cases where such events had previously happened recurrently. |
|||||||||||||||||||||||||||||||||||||
|
|
Classification
Diagnose after official ICD-10 Classification |
|||||||||||||||||||||||||||||||||||||
|
|
AddressesWe have a list of obstetrical departments and clinics mainly in German speaking countries where – as far as we know – Early Total Cervix Occlusions are performed. We are taking trouble to get hold of more addresses. If a clinic performing this operation is not included in the list, or certain changes may have taken place, please let us know. |
|||||||||||||||||||||||||||||||||||||
|
|
Video about TCOThe complete course of the operation of the Total Cervix Occlusion is available for a small fee in the form of a self-made video with a commentary in German or English. The amount that exceeds the production costs benefit the non-profit making Erich Saling-Institute of Perinatal Medicine.
|
|||||||||||||||||||||||||||||||||||||
|
|
References
|
|||||||||||||||||||||||||||||||||||||